Science Fact Friday: Tetrodotoxin, Ft. A Small Gif Because I’m Avoiding My Real Obligations. Why Does

Science Fact Friday: Tetrodotoxin, ft. a small gif because I’m avoiding my real obligations. Why does tetrodotoxin not affect its host? More studies need to be done but at least a few species possess mutated sodium ion channels. The tetrodotoxin can’t interact efficiently with the altered channels.
Another interesting tidbit: Animals with tetrodotoxin can lose their toxicity in captivity. It is suspected that the animals accumulate the toxic bacteria as a side-effect of their diet. After several years of captivity on a tetrodotoxin-bacteria-free diet, the bacterial colonies living in the animals die, residual toxin is cleared from the system, and the animal is safe to handle.
More Posts from Contradictiontonature and Others


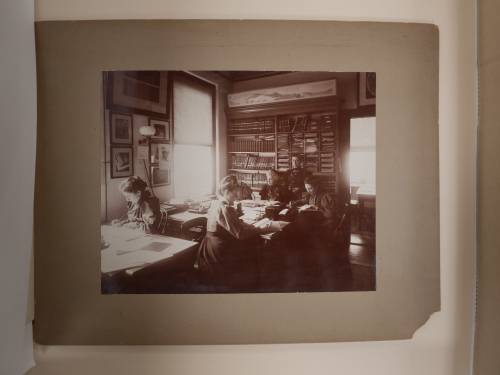
This team of early female astronomers created the star classification system we use today.
In the late 19th century, astronomy was a growing field. At the time, Edward Pickering, the director of the Harvard College Observatory, was working to create a classification system for stars by capturing the light from these distant celestial objects onto photographic glass plates. A team of female assistants and astronomers meticulously maintained and analyzed these delicate negatives. In her new book, The Glass Universe: How the Ladies of the Harvard Observatory Took the Measure of the Stars, Dava Sobel shares the stories of these female “human computers” and how their work helped to advance the field of astronomy and the role of women in science.
This team of astronomers included Williamina Fleming, who was once Pickering’s maid but eventually became a supervisor to the group and went on to identify hundreds of variable stars. And Henrietta Swan Leavitt’s observations about the luminosity of stars would shape later ideas about the expanding universe.
Listen to the interview here.
[Photos courtesy of The Glass Universe]

Collective memory in bacteria
Individual bacterial cells have short memories. But groups of bacteria can develop a collective memory that can increase their tolerance to stress. This has been demonstrated experimentally for the first time in a study by Eawag and ETH Zurich scientists published in PNAS.
Roland Mathis, Martin Ackermann. Response of single bacterial cells to stress gives rise to complex history dependence at the population level. PNAS, March 7, 2016 DOI: 10.1073/pnas.1511509113
Experimental set-up with the bacterium Caulobacter crescentus in microfluidic chips: each chip comprises eight channels, with a bacterial population growing in each channel. The bacteria are attached to the glass surface by an adhesive stalk. When the bacterial cells divide, one of the two daughter cells remains in the channel, while the other is washed out. Using time-lapse microscopy, bacterial cell-division cycles and survival probabilities can thus be reconstructed. Credit: Stephanie Stutz

A French man who lives a relatively normal, healthy life - despite missing 90 percent of his brain - is causing scientists to rethink what it is from a biological perspective that makes us conscious.
Despite decades of research, our understanding of consciousness - being aware of one’s existence - is still pretty thin. We know that it’s somehow based in the brain, but then how can someone lose the majority of their neurons and still be aware of themselves and their surroundings?
First described in The Lancet in 2007, the case of the man with the missing brain has been puzzling scientists for almost 10 years.
Read more…
Molecule of the Day: VX


VX (C11H26NO2PS) is a colourless, odourless, oily liquid under room temperatures. It is a member of the V-series of nerve agents, and is an extremely potent poison - only 0.01 grams of it is needed to kill a person by skin contact. VX was recently implicated in the assassination of Kim Jong-nam, the half-brother of the North Korean leader Kim Jong-un, in Malaysia.
VX is a potent inhibitor of acetylcholinesterase, which breaks down the neurotransmitter acetylcholine into acetic acid and choline. The normal function of the enzyme is to regulate the concentration of acetylcholine within the synaptic cleft, so as to control the frequency of binding of acetylcholine to cholinergic receptors on the postsynaptic cell membrane and hence the transmission of impulses across the synapse.

Consequently, the inhibition of acetylcholinesterase results in a rapid increase in the synaptic concentration of acetylcholine, as the presynaptic knob continues to synthesise it and secrete it into the synaptic cleft. As a result, the cholinergic receptors on the postsynaptic cell membrane are continually stimulated, and a rapid series of action potentials are triggered. This results in muscle spasms and eventual paralysis, leading to death by asphyxiation due to paralysis of the diaphragm.

VX exposure is usually treated using an injection of atropine and pralidoxime. Atropine inhibits certain cholinergic receptors, reducing the binding of acetylcholine to receptors and thus the triggering of action potentials. On the other hand, one end of pralidoxime binds to acetylcholinesterase and the other binds to the phosphate group of VX, which causes the VX molecule to detach from the enzyme together with the pralidoxime molecule (see below). This restores the ability of acetylcholinesterase to hydrolyse acetylcholine, hence reducing its synaptic levels.

VX is synthesised from phosphorus trichloride over multiple steps; first, it is methylated, reacted with ethanol, then transesterified with N,N-diisopropylaminoethanol to produce QL. This is then oxidised with sulfur, and isomerised via heating to produce VX.

Phenyllithium or lithobenzene is an organometallic agent with the empirical formula C6H5Li. Crystalline phenyllithium is colorless; however, solutions of phenyllithium are various shades of brown or red depending on the solvent. It is a highly air and moisture sensitive compound, that could be easily decomposed by any protic solvent.

In this case it was a byproduct of a synthesis of an organophosphorous compound and it was only present in a LOW concentration, therefore it was safe to decompose it by simply adding cold water. It’s important to note that it could be dangerous to decompose organometallic compounds by simply adding water. Also, in this case, the highly toxic BENZENE was the product of this reaction, what should be handled with care.

5 sleep disorders you didn’t know existed
Ever shouted at your partner while you slept, or woken up unable to move? From apnoea to exploding heads, here are some strange things that go bump in the night.
Sleep apnoea
A surprisingly common condition in which you stop breathing for 10 seconds or more as you sleep. The lack of oxygen causes your brain to wake you up, or pull you into much lighter sleep. Either way, it can have a profound effect on the quality of your sleep – and that of any bedfellow, as it’s often accompanied by loud snoring.
Sleep paralysis
A terrifying experience, where the body, which naturally becomes paralysed duringREM sleep, is still paralysed when you wake. You are fully conscious but cannot move or speak, sometimes for several minutes. Some people also feel as if they are choking or their chest is being crushed and they may have visual hallucinations. The condition can be exacerbated by sleep deprivation, some drugs, and disorders such as sleep apnoea.
Hypnagogic jerks
Those jumps or twitches you experience as you nod off, often accompanied by the sensation of falling. The cause remains a mystery. One idea is that you start dreaming before your body becomes paralysed. Another is that the twitches are a by-product of your nervous system relaxing as you drift off.
REM sleep disorder
If you’ve ever punched or shouted at your partner in the night, only to remember nothing next morning, you may have been in the grip of this condition. Here, the body isn’t fully paralysed during REM sleep, so people act out their dreams. Thistends to happen only with bad dreams.
Exploding head syndrome
This entails the sensation of a loud noise, like an exploding bomb or a gunshot, as you drift off or wake up. It affects about 1 in 10 of us and it tends to start around age 50. Nobody knows what causes it– perhaps physical changes in the middle ear, or a minor seizure in the brain’s temporal lobe. Despite its name, the condition is harmless.
Image Credit: Toby Leigh
Source: New Scientist (By Catherine de Lange)

It’s #InternationalWomensDay! Here are twelve pioneering female chemists. Larger image & downloadable poster: http://wp.me/p4aPLT-2ra

After the heart is “cleansed of blood and all cells”, only connective tissues remain. This is ideal for doing heart transplants because the recipient’s immune system is less likely to reject the ghost heart if it has no trances of the donor’s body. [Image via http://bit.ly/2izEnse]

A New Way to Cross the Blood–Brain Barrier - A Mental Unblock
The brain presents a unique challenge for medical treatment: it is locked away behind an impenetrable layer of tightly packed cells. Although the blood-brain barrier prevents harmful chemicals and bacteria from reaching our control center, it also blocks roughly 95 percent of medicine delivered orally or intravenously. As a result, doctors who treat patients with neurodegenerative diseases, such as Parkinson’s, often have to inject drugs directly into the brain, an invasive approach that requires drilling into the skull.
Some scientists have had minor successes getting intravenous drugs past the barrier with the help of ultrasound or in the form of nanoparticles, but those methods can target only small areas. Now neuroscientist Viviana Gradinaru and her colleagues at the California Institute of Technology show that a harmless virus can pass through the barricade and deliver treatment throughout the brain.
Gradinaru’s team turned to viruses because the infective agents are small and adept at entering cells and hijacking the DNA within. They also have protein shells that can hold beneficial deliveries, such as drugs or genetic therapies. To find a suitable virus to enter the brain, the researchers engineered a strain of an adeno-associated virus into millions of variants with slightly different shell structures. They then injected these variants into a mouse and, after a week, recovered the strains that made it into the brain. A virus named AAV-PHP.B most reliably crossed the barrier.
Next the team tested to see if AAV-PHP.B could work as a potential vector for gene therapy, a technique that treats diseases by introducing new genes into cells or by replacing or inactivating genes already there. The scientists injected the virus into the bloodstream of a mouse. In this case, the virus was carrying genes that encoded green fluorescent proteins. So if the virus made it to the brain and the new DNA was incorporated in neurons, the success rate could be tracked via a green glow on dissection. Indeed, the researchers observed that the virus infiltrated most brain cells and that the glowing effects lasted as long as one year. The results were recently published in Nature Biotechnology.
In the future, this approach could be used to treat a range of neurological diseases. “The ability to deliver genes to the brain without invasive methods will be extremely useful as a research tool. It has tremendous potential in the clinic as well,” says Anthony Zador, a neuroscientist who studies brain wiring at Cold Spring Harbor Laboratory. Gradinaru also thinks the method is a good candidate for targeting areas other than the brain, such as the peripheral nervous system. The sheer number of peripheral nerves has made pain treatment for neuropathy difficult, and a virus could infiltrate them all.
Image Credit: Thomas Fuchs
Source: Scientific American (By Monique Brouillette)
-
 swimminginthevoid reblogged this · 8 months ago
swimminginthevoid reblogged this · 8 months ago -
 worstreligiousfanart liked this · 1 year ago
worstreligiousfanart liked this · 1 year ago -
 clayrot liked this · 1 year ago
clayrot liked this · 1 year ago -
 sgtpeppersofab liked this · 2 years ago
sgtpeppersofab liked this · 2 years ago -
 colbaltsunfire reblogged this · 2 years ago
colbaltsunfire reblogged this · 2 years ago -
 colbaltsunfire liked this · 2 years ago
colbaltsunfire liked this · 2 years ago -
 randomdemonex reblogged this · 2 years ago
randomdemonex reblogged this · 2 years ago -
 randomdemonex liked this · 2 years ago
randomdemonex liked this · 2 years ago -
 jiroyu liked this · 2 years ago
jiroyu liked this · 2 years ago -
 changeling-ash reblogged this · 2 years ago
changeling-ash reblogged this · 2 years ago -
 changeling-ash liked this · 2 years ago
changeling-ash liked this · 2 years ago -
 vintage-squid reblogged this · 2 years ago
vintage-squid reblogged this · 2 years ago -
 anastomosis liked this · 2 years ago
anastomosis liked this · 2 years ago -
 neuronium reblogged this · 2 years ago
neuronium reblogged this · 2 years ago -
 falselament liked this · 3 years ago
falselament liked this · 3 years ago -
 elielloving liked this · 3 years ago
elielloving liked this · 3 years ago -
 neuronium liked this · 3 years ago
neuronium liked this · 3 years ago -
 pakaloloblowin-blog liked this · 4 years ago
pakaloloblowin-blog liked this · 4 years ago -
 sunkissedempire liked this · 4 years ago
sunkissedempire liked this · 4 years ago -
 itscryptifssil liked this · 4 years ago
itscryptifssil liked this · 4 years ago -
 cephalopodnerd1987 liked this · 4 years ago
cephalopodnerd1987 liked this · 4 years ago -
 moonlightrisesblog liked this · 4 years ago
moonlightrisesblog liked this · 4 years ago -
 elfo8792 liked this · 5 years ago
elfo8792 liked this · 5 years ago -
 parasect reblogged this · 6 years ago
parasect reblogged this · 6 years ago -
 heresathreebee liked this · 6 years ago
heresathreebee liked this · 6 years ago -
 danny-darkness liked this · 6 years ago
danny-darkness liked this · 6 years ago -
 panda-poes reblogged this · 6 years ago
panda-poes reblogged this · 6 years ago -
 spicesfrommars reblogged this · 6 years ago
spicesfrommars reblogged this · 6 years ago -
 katbird0152 liked this · 6 years ago
katbird0152 liked this · 6 years ago -
 oreosforthecaptain liked this · 6 years ago
oreosforthecaptain liked this · 6 years ago -
 greef1 liked this · 6 years ago
greef1 liked this · 6 years ago -
 tiddyciddy liked this · 6 years ago
tiddyciddy liked this · 6 years ago -
 radioactivemangos liked this · 6 years ago
radioactivemangos liked this · 6 years ago -
 porcelainski liked this · 6 years ago
porcelainski liked this · 6 years ago -
 yesistaken liked this · 6 years ago
yesistaken liked this · 6 years ago -
 xxxxxxxxxxxsz liked this · 6 years ago
xxxxxxxxxxxsz liked this · 6 years ago -
 sweetlyminiaturesublime liked this · 6 years ago
sweetlyminiaturesublime liked this · 6 years ago -
 salakalava reblogged this · 6 years ago
salakalava reblogged this · 6 years ago -
 juoksiainen liked this · 6 years ago
juoksiainen liked this · 6 years ago -
 idkaboutnames reblogged this · 6 years ago
idkaboutnames reblogged this · 6 years ago -
 idkaboutnames liked this · 6 years ago
idkaboutnames liked this · 6 years ago -
 ssluggishh reblogged this · 6 years ago
ssluggishh reblogged this · 6 years ago -
 ssluggishh liked this · 6 years ago
ssluggishh liked this · 6 years ago -
 patternedsuitcollection reblogged this · 6 years ago
patternedsuitcollection reblogged this · 6 years ago
A pharmacist and a little science sideblog. "Knowledge belongs to humanity, and is the torch which illuminates the world." - Louis Pasteur
215 posts
